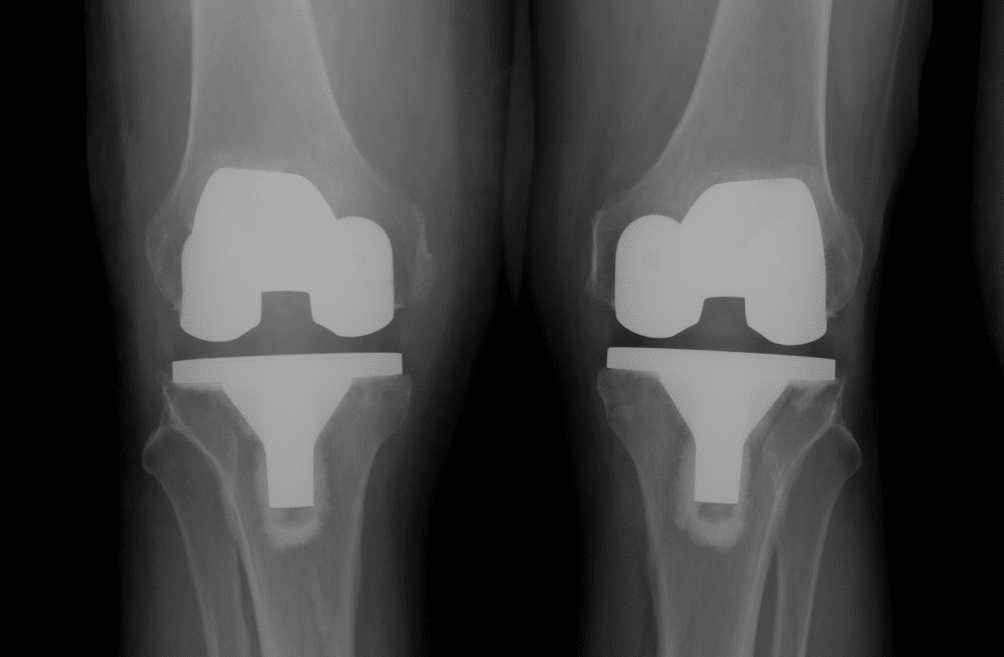
I saw a longstanding patient of mine last week for a catch up regarding his hips. I hadn’t seen him for about 3 years. He had just celebrated his 95th birthday and is still living independently and very active. He told me he had retired from playing tennis a couple of years ago at 93! I had operated on him 10 years ago when he had a problem with his right hip replacement. He brought along some xrays of his hips. His right side was fine and his left hip showed a hip replacement with signs of significant socket (acetabular) wear but he had no symptoms at all. How old is that hip replacement ? – 20 years? Or more??

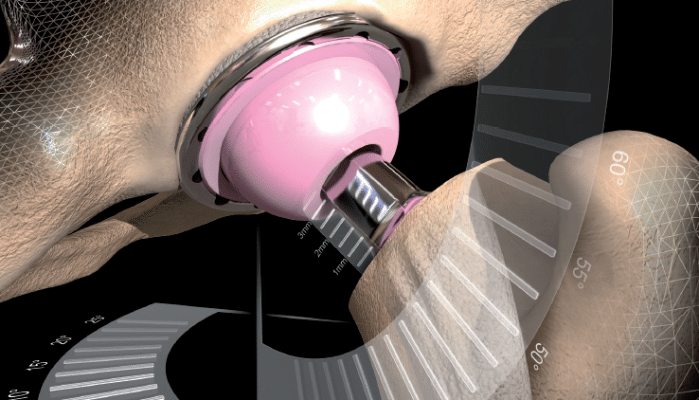
Well, his left hip was replaced in 1974 by a Melbourne surgeon, now retired. He has an original Charnley cemented one piece femoral stem/head and acetabulum undertaken through a direct lateral approach with trochanteric osteotomy, as per the operative technique described by Charnley for his Low Friction Arthroplasty (LFA). We would consider this LFA nowadays to be the prototype of all modern hip replacement implants, undertaken using what would now be considered fairly primitive cementing and surgical techniques. It is 42 years old and aside from the wear, the implant itself looks solidly fixed to bone. An amazing result for a metal on polyethylene bearing, particularly given that the Charnley LFA is a small metal head (22.2mm stainless steel head) articulating with an (unadulterated, non-crosslinked) all polyethylene socket. This hip replacement was undertaken in a man of 53 years who has led an active life including playing sport – certainly a very good test for any hip replacement and its articulating surfaces. This got me thinking about joint replacement bearing surfaces. What is the best bearing surface and particularly what is the best bearing surface for a younger active patient undergoing hip replacement?

The reality is – there is no ideal surface, just advantages and disadvantages to each coupling. An ideal bearing surface would be one where the wear is minimal and the wear debris particles generated cause no local or systemic problem. If such a surface was available then joint replacements could last the term of one’s natural life, irrespective of activity level.
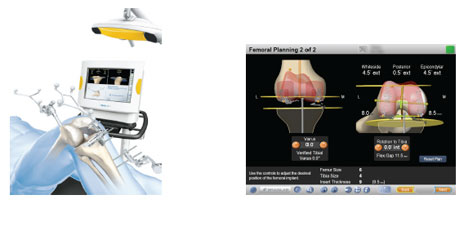
There are multiple factors influencing implant longevity. The first of these is naturally the age and life expectancy of the recipient. The activity level and weight of the patient are very significant factors. Traditionally young active patients have a far greater chance of requiring revision hip replacement surgery. The implant itself is a factor but questionably the most important factor may be the choice of implant bearing surface. The alignment of the bearing surfaces at the time of surgery will influence longevity – it has been well documented that poor alignment leads to edge loading and excessive wear on any surface.
Tribology is the science associated with the study of surfaces interacting under load and incorporates the concepts of friction, wear and lubrication. The pursuit of excellence in bearing surface technology has led to a number of alternative bearing surface couplings being available in total hip replacement surgery. The surfaces commonly used include “soft” bearings such as metal or ceramic on polyethylene and “hard” bearings like metal on metal or ceramic on ceramic.
Figure 2. Wear rates of different hip replacement bearing surfaces.
Metal on poly (MoP) is the most commonly used surface in hip replacement surgery. Modern day polyethylene is generally cross-linked and this has reduced surface/particulate wear to about 10% of that seen with original untreated poly. MoP surfaces are durable, versatile and have a long, successful and well researched history. The particulate wear is not toxic but can be associated with osteolysis and late aseptic loosening. Ceramic on poly has slightly less wear than MoP but does have a bedding in period and some issues associated with ceramics.
Metal on metal (MoM) surfaces have been around since the 60’s with the McKee Farrar and Ring prostheses. They had issues with with high rates of loosening, being largely abandoned in the late 70’s. MoM underwent a resurgence in the late 90’s with both conventional and resurfacing type hip replacements. These surfaces are generally made of a highly polished cobalt/chromium alloy. MoM interfaces show low rates of wear compared with MoP, but despite this, the number of particles generated each year is about 14,000x more than an equivalent polyethylene surface. These tiny sub-micron particles accumulate in the bone and soft tissue surrounding the implant and in susceptible individuals can lead to a hypersensitivity tissue reaction. If this occurs early aseptic loosening of the implant ensues often with significant bone and soft tissue destruction or pseudotumour formation. In some patients increased serum levels of cobalt and chromium ions can reach toxic levels with deposition in liver, kidney and central nervous systems and unknown long term effects.
Ceramic on ceramic (CoC) articulations are potentially high performing surfaces with the least wear of any bearing surface. Similar to polyethylene, particulate debris is not generally toxic but can still be associated with aseptic loosening. Ceramic does have an incidence of fracture with potentially sudden catastrophic failure and is associated with up to a 20% incidence of implant “squeaking” with movement. Poorly sited CoC implants with edge loading can lead to “chipping” and the generation of large ceramic shards or fragments. If a CoC surface needs to be revised for any reason it is generally accepted that the same surface needs to used again. This is because of the potential abrasiveness of ceramic particles creating 3rd body wear (accelerated wear from particles inside an articulation scratching the surface with movement).
In general, “hard” bearings wear less and should last longer but are more expensive and less forgiving. They require more precise implant placement to reduce impingement and edge loading and risk of fracture. “Soft” bearings are more forgiving and cross-linked polyethylene now has excellent clinical results out to nearly 20 years.
I’m pretty conservative in my practice and almost exclusively use metal on x-linked polyethylene for all patients, including younger more active individuals undergoing hip replacement surgery. It is the bearing surface I feel most comfortable with. It has excellent longevity, is unquestionably the safest articulation and if revision surgery is required it does not limit future alternative bearing surface options.