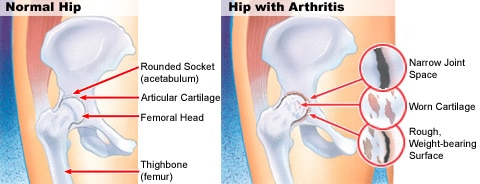
Hip Osteoarthritis, like all forms of arthritis, is due to a loss of the cushioning joint surface tissue (articular cartilage) that covers the ends of the bones of the joint – the femoral head (ball) and the acetabulum of the pelvis (socket). This is a progressive condition and the natural history is one of slow deterioration – as the articular cartilage loss increases, so usually do the symptoms. When the articular cartilage layers are worn away completely, the joint articulates with “bone on bone” surfaces – this is usually very painful (as the bone has lots of nerve endings) and constitutes an advanced osteoarthritis. Osteoarthritis differs from inflammatory arthritis in that the articular cartilage loss is due to “wear and tear” (a degenerative process – osteoarthritis is also known as degenerative arthritis) rather than due to an inflammatory process.
In most cases hip osteoarthritis is idiopathic (primary hip OA) – this means that there is no identifiable reason as to why it has arisen. Clearly as we get older there tends to be more natural wear of the joint surfaces (similar to the tread on a car tyre) but some hips never become arthritic despite advanced age. Presumably this has to do with the durability of the articular cartilage, which is probably genetically predetermined. Interestingly hip osteoarthritis can run in families. Similar to the car tyre analogy, lots of activity (driving) may predispose some individuals to more joint surface wear. It has been established for some time now that obesity is a major risk factor for the development of lower limb joint arthritis – there are both excessive load and chemical theories for this.
In some cases there are clearly identifiable reasons why osteoarthritis has occurred (secondary hip OA). The car tyre analogy here is that tread wear is more significant when the wheel balancing is poor. Predisposing conditions include congenital abnormalities of the hip (dysplasia or dislocation) which have affected the growth and shape of the ball or socket leading to abnormal and excessive wear. Conditions affecting the growth of the hip in childhood (eg Perthes disease or Slipped Upper Femoral Epiphysis) also alter the shape of the hip. Injury to the hip like a traumatic dislocation can damage the joint surface directly starting the wear process. Conditions such as osteochondritis can lead to joint surface damage and secondary OA.
In recent years, a condition called Femoroacetabular Impingement (FAI) has been recognized as a possible cause for osteoarthritis – it is thought to be a factor in some cases of primary hip OA, where previously no other cause had been identified. Again FAI is caused by subtle changes in the shape of the ball and socket leading to a slight joint surface mismatch, which over a long period of time is thought to lead to joint surface wear. Over the next decade long term studies should be able to determine whether this is the case and whether treating FAI in its early stages may prevent arthritis developing in patients with this condition.
The main symptom/complaint with hip osteoarthritis is pain. This is usually located in the groin or the front part of the hip and can sometimes be misdiagnosed early as a “groin strain”. There can be pain that radiates down the front of the thigh to the level of the knee. Occasionally patients with hip arthritis will present mainly with pain around the knee – this is obviously confusing for everyone concerned. Pain located mainly in the buttock or the back of the thigh is rarely due to hip arthritis. In most cases, the pain comes on gradually without an obvious injury or incident. At the start the pain may only occur with or after heavy physical exertion like running, but as the condition progresses the pain may be felt with normal day to day walking and when end stage is often felt at rest. Patients will often notice difficulty bending down to put on socks and shoes and attend to toenails and often have difficulty getting in and out of the car.
Hip osteoarthritis is often diagnosed on the basis of history and clinical examination. It is usually easily confirmed on plain xray, but sometimes more extensive investigations like MRI scan can be helpful particularly in the early stages of the condition.
Hip osteoarthritis is a complex condition and there are no treatments that will reverse the joint surface wear changes once they have started to take place. The treatment or management of osteoarthritis of the hip needs to be tailored to each individual depending on the severity of the condition and how this is affecting the person afflicted. In the early phases of this condition when the symptoms are mild, conservative or non-operative treatment is usually recommended. Conservative management principles centre around education of the condition, activity and lifestyle modification, weight reduction, the use of physical aids and the careful use of medication for symptom reduction or relief. These measures are about making it easier to manage with the symptoms (usually pain and stiffness) on a “day to day” basis.
Operative management or surgery for osteoarthritis of the hip is really only indicated for end stage “bone on bone” joint surfaces. Surgery for early or middle stage disease in most cases does not significantly improve symptoms or function. Total Hip Replacement (THR) is generally the treatment of choice for advanced hip osteoarthritis with unmanageable pain and very significant impairment of function (ability to walk, bend and undertake simple activities of daily living). It should be noted that THR is a compromise operation and will never provide the recipient with a completely normal hip. THR is however generally very successful in providing significant pain relief and restoration of function in a significantly impaired individual with end stage disease.
Source: https://www.parkclinic.com.au/osteoarthritis-of-the-hip/